RESUMO
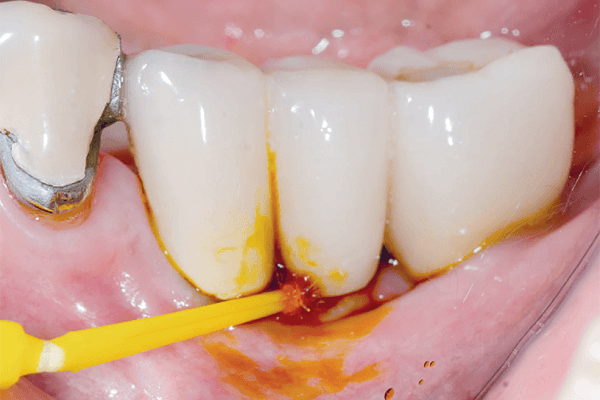
O objetivo deste relato de caso clínico foi ilustrar uma proposta de tratamento de peri-implantite. Paciente do sexo feminino, com 71 anos de idade, saudável, não fumante, procurou a clínica com queixa de dor e sangramento na região do implante que estava em função há três anos. Após exame clínico e radiográfico, verificou-se que o implante na região do dente 44 apresentava sinais clínicos e radiográficos característicos de peri-implantite. Foi realizado tratamento não cirúrgico, com orientação de higiene oral, desorganização do biofilme e, posteriormente, o tratamento cirúrgico com debridamento mecânico da superfície do implante, descontaminação local com tetraciclina e colocação de enxerto ósseo xenógeno associado ao enxerto de tecido conjuntivo subepitelial. Após um mês, constatou-se a eliminação do processo inflamatório e o restabelecimento da morfologia dos tecidos peri-implantares, mantendo-se desta forma durante os 18 meses de acompanhamento. É válido ressaltar que o estabelecimento de terapia periodontal de suporte rigorosa foi primordial para o sucesso a longo prazo.
Palavras-chave – Implantes dentários; Peri-implantite; Mucosite.
ABSTRACT
The objective of this clinical case report is to illustrate a proposed treatment for peri-implantitis. A female, 71 years-old, healthy, and non-smoker patient, came to the clinic complaining of pain and bleeding in the region of the implant that had been in use for 3 years. After clinical and radiographic examination, it was found that the implant in the region of tooth 44 presented clinical and radiographic signs characteristic of peri-implantitis. Non-surgical treatment was carried out, with guidance on oral hygiene, disorganization of the biofilm and subsequently, surgical treatment with mechanical debridement of the implant surface, local decontamination with tetracycline and placement of a xenogeneic bone graft associated with the subepithelial connective tissue graft. After 1 month, the inflammatory process was eliminated and the morphology of the peri-implant tissues was restored, remaining this way for 18 months of follow-up. It is worth noting that the establishment of rigorous supportive periodontal therapy was paramount to long-term success.
Key words – Dental implants; Peri-implantitis; Mucositis.
Referências
- Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res 2007;18(6):669-79.
- Renvert S, Polyzois I. Treatment of pathologic peri-implant pockets. Periodontol 2000 2018;76(1):180-90.
- Bianchini MA, Claus JDP. Diagnóstico das alterações peri-implantares. In: Diagnóstico e tratamento das alterações peri-implantares (1a). São Paulo: Santos, 2014. p.1-16.
- Fransson C, Wennström J, Berglundh T. Clinical characteristics at implants with a history of progressive bone loss. Clin Oral Implants Res 2008;19(2):142-7.
- Ferreira RCQ, Kuguimyia RN, Rodrigues RA, Lins RAU, Dias AHM, Gade-Neto CR. Abordagem clínica da peri-implantite. Rev Bras Implantodon Prótese Implant 2006;13(51):150-4.
- Quirynen M, Herrera D, Teughels W, Sanz M. Implant therapy: 40 years of experience. Periodontol 2000 2014;66(1):7-12.
- Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS et al. A new classification scheme for periodontal and peri-implant diseases and conditions – introduction and key changes from the 1999 classification. J Clin Periodontol 2018;45:45(suppl.20):S1-S8.
- Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions. J Clin Periodontol 2018;45(suppl.20):S286-91.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Clin Periodontol 2018;45(suppl.20):S246-66.
- Renvert S, Polyzois IN. Clinical approaches to treat periimplant mucositis and peri-implantitis. Periodontol 2015;68(1):369.
- Salvi GE, Cosgarea R, Sculean A. Prevalence and mechanisms of peri-implant diseases. J Dent Res 2017;96(1):31-7.
- Figuero E, Graziani F, Sanz I, Herrera D, Sanz M. Management of peri-implant mucositis and peri-implantitis. Periodontol 2014;66(1):255-73.
- Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000 1998;17:63-76.
- Sanz-Martin I, Doolittle-Hall J, Teles RP, Patel M, Belibasakis GN, Hammerle CHF et al. Exploring the microbiome of healthy and diseased peri-implant sites using Illumina sequencing. J Clin Periodontol 2017;44(12):1274-84.
- Kröger A, Hulsmann C, Fickl S, Spinell T, Hutti F, Kaufmann F et al. The severity of human peri-implantitis lesions correlates with the level of submucosal microbial dysbiosis. J Clin Periodontol 2018;45(12):1498-509.
- Lang NP, Bosshardt DD, Lulic M. Do mucositis lesions around implants differ from gingivitis lesions around teeth? J Clin Periodontol Denmark 2011;38(suppl.11):182-7.
- Lang NP, Salo A, Kontio R, Ylijoki S, Lindqvist C, Suuronen R. Failed dental implants – clinical, radiological and bacteriological findings in 17 patients. J Craniomaxillofac Surg 2000;33(3):212-7.
- Lee C-T, Huang Y-W, Zhu L, Weltman R. Prevalences of peri-implantitis and peri-implant mucositis: systematic review and meta-analysis. J Dent 2017;62:1-12.
- Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL et al. Impact of maintenance therapy for the prevention of peri-implant diseases: a systematic review and meta-analysis. J Dent Res 2016;95(4):372-9.
- Saaby M, Karring E, Schou S, Isidor F. Faxtors influencing severity of peri-implantitis. Clin Oral Implants 2016;27(1):7-12.
- Froum SJ, Rosen PS. A proposed classification for peri-implantitis. Int J Periodontics Restorative Dent 2012;32(5):533-540.
- Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol 2017;44(5):456-62.
- Kumar PS, Mason MR, Brooker MR, O’Brien K. Pyrosequencing reveals unique microbial signatures associated with healthy and failing dental implants. J Clin Periodontol 2012;39(5):425-33.
- Carcuac O, Derks J, Abrahamsson I, Wennström JL, Petzold M, Berglundh T. Surgical treatment of peri-implantitis: 3- year results from a randomized controlled clinical trial. J Clin Periodontol 2017;44(12):1294-303.
- Heitz-Mayfield LJA, Salvi GE, Mombelli A, Loup PJ, Heitz F, Kruger E et al. Supportive peri-implant therapy following anti-infective surgical peri-implantitis treatment: 5-year survival and success. Clin Oral Implants Res 2018;29(1):1-6.
- Salvi R, Cosgarea R, Sculean A. Prevalence and mechanisms of peri-implant diseases. J Dent Res 2017;96(1):31-7.
- Sarmiento HL, Norton MR, Fiorellini JP. A classification system for peri-implant diseases and conditions. Int J Periodontics Restorative Dent 2016;36(5):699-705.
- Brignardello-Petersen R. Insufficient evidence about benefits of antimicrobial photodynamic therapy as an adjunct to mechanic curettage in smokers with peri-implant mucositis. J Am Dent Assoc 2017;148(8):e114.
- Pompa CC, Ribeiro EDP, Sousa SB. Peri-implantite: diagnóstico e tratamento. Innov Implant J Biomater Esthet 2009;4(1):52-7.
- Tagliari D, Takemoto M, de Andrade MR. Tratamento da peri-implantite: revisão de literatura. Revista Tecnológica 2015;3(2):68-77.