Relato de caso tem como objetivo demonstrar a viabilidade e eficácia da ROG em defeito ósseo vertical e horizontal.
RESUMO
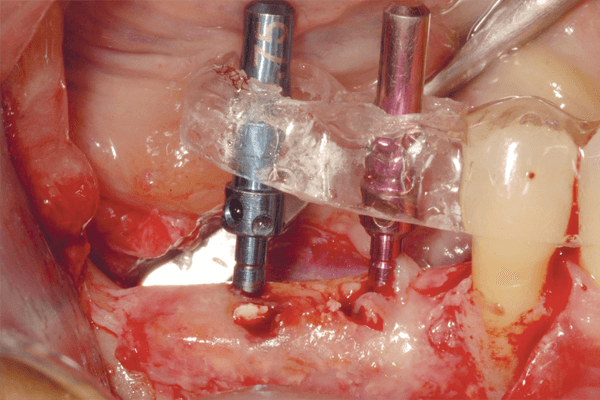
O objetivo deste relato de caso foi demonstrar a viabilidade e efi cácia da ROG em defeito ósseo vertical e horizontal. Paciente do sexo feminino, com 62 anos de idade e sem comorbidades, compareceu ao Instituto Opem com queixa principal de “difi culdade mastigatória”. Após avaliação clínica e imaginológica, identifi cou-se atrofi a óssea na região posterior de mandíbula no lado direito. O tratamento proposto foi ROG para aumento vertical e horizontal, com instalação de parafusos tenda, biomaterial xenógeno e tecido ósseo autógeno particulados (1:1) aglutinados com I-PRF, seguido da estabilização da membrana de PTFE e recobrimento da mesma com matrizes autólogas de L-PRF para oclusão da ferida cirúrgica. Foi realizado controle clínico e imaginológico com sete meses, e reabertura da área enxertada com instalação de implantes de conexão morse na região dos dentes 45 e 46, com nove meses de pós-operatório. Os implantes foram reabertos após quatro meses, seguido da instalação dos cicatrizadores e enxerto gengival livre para melhorar a qualidade da mucosa peri-implantar. Posteriormente, os minipilares foram instalados para confecção da prótese fi xa sobre implantes. Observou-se aumento vertical e horizontal expressivo na região posterior de mandíbula, possibilitando a instalação de implantes em um posicionamento tridimensional favorável à reabilitação protética, restabelecendo a função e estética, mostrando ser um procedimento viável e previsível após 44 meses de acompanhamento.
Palavras-chave – Regeneração óssea guiada; Implantes dentários; Enxerto ósseo.
ABSTRACT
The objective of this case report is to demonstrate the feasibility and eff ectiveness of GBR in vertical and horizontal bone defects. A 62-year-old female patient, without comorbidities, came to the Opem Institute with a main complaint of “masticatory diffi culty”. Aft er clinical and imaging evaluation, bone atrophy was identifi ed in the posterior mandibular right side. The proposed treatment was GBR for vertical and horizontal augmentation with the installation of tent screws, xenogenous biomaterial and particulate autogenous bone tissue (1:1) agglutinated with I-PRF, followed by stabilization of the PTFE membrane and covering it with autologous L-PRF matrices for occlusion of the surgical wound. Clinical and imaging control was performed at 7 months, and the graft ed area was reopened to receive Morse connection dental implants in the regions of teeth 45 and 46, nine months later. Then, the dental implants were reopened aft er four months, followed by installation of healing cap devices and free gingival graft to improve the quality of the peri-implant mucosa. Subsequently, the mini-abutments were installed to fabricate an implant-supported partial fi xed prosthesis. An expressive vertical and horizontal increase was observed in the posterior mandibular region, allowing the installation of dental implants in a three-dimensional approach favorable to the prosthetic rehabilitation, restoring function and aesthetics, being a viable and predictable procedure.
Key words – Guided bone regeneration; Dental implants; Bone graf
Referências
- Urban IA, Montero E, Monje A, Sanz-Sanchez I. Effectiveness of vertical ridge augmentation interventions: a systematic review and meta-analysis. J Clin Periodontol 2019;46(suppl.21):319-39.
- Bassi APF, Bizelli VF, Francatti TM, Ferreira ACRM, Carvalho Pereira J, Al-Sharani HM et al. Bone regeneration assessment of polycaprolactone membrane on critical-size defects in rat calvaria. Membranes (Basel) 2021;11(2):124.
- Keestra JA, Barry O, Jong L, Wahl G. Long-term effects of vertical bone augmentation: a systematic review. J Appl Oral Sci 2016;24(1):3-17.
- Wikesjö UM, Qahash M, Thomson RC, Cook AD, Rohrer MD, Wozney JM et al. Space-providing expanded polytetrafluoroethylene devices define alveolar augmentation at dental implants induced by recombinant human bone morphogenetic protein 2 in an absorbable collagen sponge carrier. Clin Implant Dent Relat Res 2003;5(2):112-23.
- Rangert B, Sennerby L, Meredith N, Brunski J. Design, maintenance and biomechanical considerations in implant placement. Dent Update 1997;24(10):416-20.
- Tonella BP, Pellizzer EP, Falcón-Antenucci RM, Ferraço R, Almeida DAF. Photoelastic analysis of biomechanical behavior of single and multiple fixed partial prostheses with different prosthetic connections. J Craniofac Surg 2011;22(6):2060-3.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 2003;23(4):313-23.
- Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg 1988;17(4):232-6.
- Moraes Jr. EF, Bizelli VF, Tonin AC, de Carvalho EBS. Enxerto ósseo xenógeno interposicional na região anterior de mandíbula para aumento vertical do rebordo e posterior reabilitação implantossuportada. ImplantNewsPerio 2019;4(4):686-97.
- Simion M, Jovanovic SA, Trisi P, Scarano A, Piattelli A. Vertical ridge augmentation around dental implants using a membrane technique and autogenous bone or allografts in humans. Int J Periodontics Restorative Dent 1998;18(1):8-23.
- Lim G, Lin GH, Monje A, Chan HL, Wang HL. Wound healing complications following guided bone regeneration for ridge augmentation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 2018;33(1):41-50.
- Danieletto-Zanna CF, Bizelli VF, Ramires GADA, Francatti TM, de Carvalho PSP, Bassi APF. Osteopromotion capacity of bovine cortical membranes in critical defects of rat calvaria: histological and immunohistochemical analysis. Int J Biomater 2020;2020:6426702.
- Moraes Jr. EF, de Carvalho EBS. Regeneração óssea guiada vertical e horizontal na região anterior de mandíbula associada á I-PRF e matriz de L-PRF, e posterior reabilitação implantossuportada. ImplantNews 2020;5(6):960-6.
- Moraes Jr. EF, dos Santos AC, Bizelli VF. Remoção de implante mal posicionado e correção de complicação estética com regeneração óssea guiada vertical, com tela de titânio e rotação de enxerto de tecido conjuntivo. ImplantNewsPerio 2019;4(2):314-22.
- Cucchi A, Sartori M, Aldini NN, Vignudelli E, Corinaldesi G. A proposal of pseudo-periosteum classification after GBR by means of titanium reinforced d-PTFE membranes or titanium meshes plus crosslinked collagen membranes. Int J Periodontics Restorative Dent 2019;39(4):157-65.
- Bosco AF, Bosco JM. An alternative technique to the harvesting of a connective tissue graft from a thin palate: enhanced wound healing. Int J Periodontics Restorative Dent 2007;27(2):133-9.
- Oliver RC, Löe H, Karring T. Microscopic evaluation of the healing and revascularization of free gingival grafts. J Periodontal Res 1968;3(2):84-95.
- Nobuto T, Imai H, Yamaoka A. Microvascularization of the free gingival autograft. J Periodontol 1988;59(10):639-46.
- Windisch P, Orban K, Salvi GE, Sculean A, Molnar B. Vertical-guided bone regeneration with a titanium-reinforced d-PTFE membrane utilizing a novel split-thickness flap design: a prospective case series. Clin Oral Investig 2021;25(5):2969-80.
- Saletta JM, Garcia JJ, Carames JMM, Schliephake H, da Silva Marques DN. Quality assessment of systematic reviews on vertical bone regeneration. Int J Oral Maxillofac Surg 2019;48(3):364-72.
- Urban IA, Jovanovic SA, Lozada JL. Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Int J Oral Maxillofac Implants 2009;24(3):502-10.
- Naung NY, Shehata E, Van Sickels JE. Resorbable versus nonresorbable membranes: when and why? Dent Clin North Am 2019;63(3):419-43.
- Soldatos NK, Stylianou P, Koidou VP, Angelov N, Yukna R, Romanos GE. Limitations and options using resorbable versus nonresorbable membranes for successful guided bone regeneration. Quintessence Int 2017;48(2):131-47.
- Cucchi A, Vignudelli E, Napolitano A, Marchetti C, Corinaldesi G. Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial. Clin Implant Dent Relat Res 2017;19(5):821-32.
- Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V et al. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 2017;21(6):1913-27.
- Solakoglu Ö, Heydecke G, Amiri N, Anitua E. The use of plasma rich in growth factors (PRGF) in guided tissue regeneration and guided bone regeneration. A review of histological, immunohistochemical, histomorphometrical, radiological and clinical results in humans. Ann Anat 2020;231:151528.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJJ, Mouhyi J et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101(3):37-44.
- de Obarrio JJ, Araúz-Dutari JI, Chamberlain TM, Croston A. The use of autologous growth factors in periodontal surgical therapy: platelet gel biotechnology – case reports. Int J Periodontics Restorative Dent 2000;20(5):486-97.
- Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85(6):638-46.
- Mourão CFAB, de Mello-Machado RC, Javid K, Moraschini V. The use of leukocyte- and platelet-rich fibrin in the management of soft tissue healing and pain in post-extraction sockets: a randomized clinical trial. J Craniomaxillofac Surg 2020;48(4):452-7.