Estudo avalia a distribuição das tensões em implantes com conexões internas que apresentam características geométricas diferentes.
AUTORES
Gabriel Goetten
Mestre em Implantodontia – Faculdade São Leopoldo Mandic. Orcid: 0000-0002-2343-3840.
Bruno Salles Sotto Maior
Doutor em Prótese Dental e professor do Depto. de Clínica Odontológica – Universidade Federal de Juiz de Fora. Orcid: 0000-0002-9462-0299.
Alexandre Marcelo de Carvalho
Doutor em Implantodontia – Faculdade São Leopoldo Mandic; Professor – UniFagoc/Centro Universitário Ozanan Coelho. Orcid: 0000-0001-8080-8314.
Ricardo Moreno Bonilha Neto
Doutor em Implantodontia e professor de Implantodontia – Faculdade São Leopoldo Mandic. Orcid: 0000-0001-7119-6141.
Karine Carvalho Couto
Graduada em Odontologia – Uniavan; Técnica em prótese dentária – Núcleo Avançado de Estudos Odontológicos. Orcid: 0000-0001-7734-9911.
RESUMO
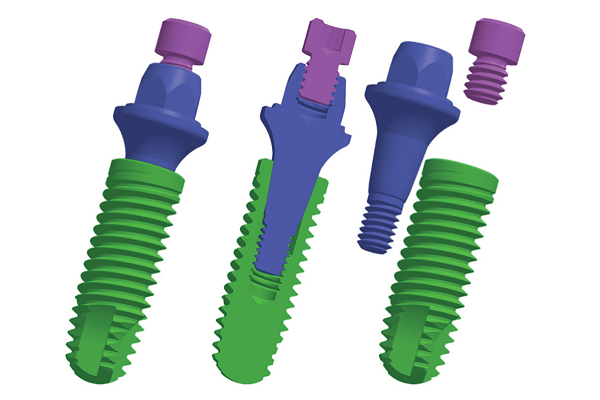
Objetivo: avaliar a distribuição das tensões em implantes com conexões internas que apresentam características geométricas diferentes, com angulações de 11,5º e 16º, através do método de análise de elementos finitos. Material e métodos: modelo M1: tratamento com implante cone-morse com angulação de 11,5º. Modelo M2: tratamento com implante cone-morse com angulação de 16º. Para simulação das cargas mastigatórias, a carga axial foi aplicada com intensidade de 100 N no sentido do longo eixo do implante; para a carga oblíqua, a intensidade foi de 100 N em 45º no sentido palatino vestibular em relação ao longo eixo do implante. Resultados: na análise do osso cortical, as maiores tensões foram para o grupo M2. A tensão nos implantes e pilares foi maior para o grupo M1, em comparação ao grupo M2. Na análise biomecânica dos parafusos, a tensão foi menor para o grupo M2. Nas coroas unitárias, os resultados quantitativos mostraram uma variação de tensão maior no grupo M1, em comparação ao grupo M2. Conclusão: as diferenças de tensão sugerem que o sistema com conicidade de 11,5º (M1) apresentou maiores picos de tensão no implante, pilar, parafuso e coroa protética, quando comparado ao sistema com conicidade 16º (M2). As tensões de tração e compressão no osso adjacente foram menores no grupo M1, com conicidade de 11,5º.
Palavras-chave – Implante dental; Interface implante-pilar; Elementos finitos; Conexão interna.
ABSTRACT
Objective: to evaluate the stress distribution in implants with internal connections that have different geometric characteristics, with angulations of 11.5 and 16 degrees using the finite element analysis method. Material and methods: model M1: treatment with a Morse Cone implant at an angle of 11.5. Model M2: treatment with Morse Cone implant at 16º angle. To simulate the masticatory loads, the axial load was applied with an intensity of 100 N in the direction of the long axis of the implant and for the oblique load, the intensity was 100 N at 45 degrees in the buccal palatal direction in relation to the long axis of the implant. Results: in the analysis of the cortical bone, the highest stresses were for the M2 group. Stress on implants and abutments was higher for group M1 compared to group M2. In the biomechanical analysis of the screws, the tension was lower for the M2 group. In the single crowns, the quantitative results showed a greater tension variation in the M1 group compared to the M2 group. Conclusion: the stress differences suggest that the system with a taper of 11.5 degrees (M1) presented higher stress peaks in the implant, abutment, screw and prosthetic crown when compared to the system with a taper of 16 degrees in the group (M2). Tensile and compressive stresses on the adjacent bone were lower in the M1 group with a taper of 11.5 degrees.
Key words – Dental implant; Implant-abutment interface; Finite elements; Internal connection.
Referências
- Eskitascioglu G, Usumez A, Sevimay M, Soykan E, Unsal E. The influence of occlusal loading location on stresses transferred to implant-supported prostheses and supporting bone: a three-dimensional finite element study. J Prosthet Dent 2004;91(2):144-50.
- Goianato MC, Shibayama R, Filho Gennari H, Medeiros RA, Pesqueira A, dos Santos DM et al. Stress distribution in implant-connection systems and cantilever lengths: digital photoelasticity. J Med Eng & Technol 2016;40(2):35-42.
- El-Anwar MI, El-Zawahry MM, Ibraheem EM, Nassani MZ, El Gabry H. New dental implant selection criterion based on implant design. Eur J Dent 2017;11(2):186-91.
- Zanardi PR, Stegun RC, Sesma N, Costa B, Shibli JA, Lagana DC. Stress distribution around dental implants placed at different depths. J Craniofac Surg 2015;26(7):2163-6.
- Carvalho MA, Sotto-Maior B, Cury A, Henrique GE. Effect of platform connection and abutment material on stress distribution in single anterior implant-supported restorations: a nonlinear 3-dimensional finite element analysis. J Prosthet Dent 2014;112(5):1096-102.
- Schmitt C, Filho-Nogueira G, Tenenbaum H, Lai J, Brito C, Doring H et al. Performance of conical abutment (morse tape) connection implants: a systematic review. J Biomed Mater Res A 2014;102(2):552-74.
- Dayrell AC, Noritomi P, Takahashi J, Consani R, Mesquita M, Santos MB. Biomechanical analysis of implant-supported prostheses with different implant-abutment connections. Int J Prosthodont 2015;28(6):621-3.
- Raoofi S, Khademi M, Amid R, Kadkhodazadeh M, Movahhedi M. Comparasion of the effect of three abutment-implant connection on stress distribution at the surface dental implants: a infinite element analysis. J Dent Res Coin Dent Prospects 2013;7(3):132-9.
- Vetromilla B, Brondani L, Pereira-Cenci T, Bergoli C. Influence of different implant-abutment connection designs on the mechanical and biological behavior of single-tooth implants in the maxillary esthetic zone: a systematic review. J Prosthet Dent 2019;121(3):398-403.
- Cehreli MC, Akça K, Iplikçioglu H, Sahin S. Dynamic fatigue resistance of implant-abutment junction in an internally notched morse-taper oral implant: influence of abutment design. Clin Oral Implants Res 2004;15(4):459-65.
- Aguirrebeitia J, Abasolo M, Vallejo J, Ansola R. Dental Implants with conical implant-abutment interface: influence of the conical angle difference on the mechanical behavior of the Implant. Int J Oral Maxillofac Implants 2013;28(2):72-82.
- Gross M, Kozak D, Laufer BZ, Weiss EI. Manual closing torque in five implant abutment systems: an in vitro comparative study. J Prosthet Dent 1999;81(5):574-8.
- Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent 2010;30(1):89-95.
- Yoo J, Moon IS, Cheng C, Yun JH, Chung C, Huh JK et al. Effect of initial placement level and wall thickness on maintenance of the marginal bone level in implants with a conical implant-abutment interface: a 5-year retrospective study. J Periodontal Implant Sci 2019;49(3):185-92.
- Caricasulo R, Malchiodi L, Ghensi P, Fantozzi G, Cucchi A. The influence of implant-abutment connection to peri-implant bone loss: a systematic review and meta-analysis. Clin Implant Dent Relat Res 2018;20(4):653-64.
- Takahashi J, Dayrell A, Consani RL, Nobilo MA, Henriques GE, Mesquita M. Stress evaluation of implant-abutment connections under different loading conditos: a 3D finite element study. J Oral Implantol 2015;41(2):133-7.
- Sotto-Maior B, Senna P, Silva W, Rocha E, Del Bel Cury A. Influence of crown-to-implant ratio, retention system, restorative material, and occlusal loading on stress concentrations in single short implants. Int J Oral Maxillofac Implants 2012;27(3):e13-8.
- Cho YS, Huh YH, Park CJ, Cho LR. Three-dimensional finite element analysis on stress distribution of internal implant-abutment engagement feature. Int J Oral Maxillofac Implants 2018;33(2):319-27.
- Yao KT, Chen CS, Cheng CK, Fang HW, Huang CH, Kao HC et al. Optimization of the conical angle design in conical implant-abutment connections: a pilot study based on the finite element method. J Oral Implantol 2018;44(1):26-35.
- Katsavochristou A, Koumolis D. Incidence of abutment screw failure of single or splinter implant prostheses: a review and update on current clinical status. J Oral Rehabil 2019;46(8):776-86.
- Rangert BR, Sullivan RM, Jemt TM. Load factor control for implants in the posterior partially edentulous segment. Int J Oral Maxillofac Implants 1997;12(3):360-70.
- Haack JE, Sakaguchi RL, Sun T, Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants 1995;10(5):529-36.
- Jorn D, Kohorst P, Besdo S, Rucker M, Stiesch M, Borchers L. Influence of lubricant on screw preload and stresses in a finite element model for a dental implant. J Prosthet Dent 2014;112(2):340-8.
- Zarb GA, Albrektsson T. Towards optimized treatment outcomes for dental implants. J Prosthet Dent 1998;80(6):63940.
- Goheen KL, Vermilyea SG, Vossoughi J, Agar JR. Torque generated by handheld screwdrivers and mechanical torquing devices for osseointegrated implants. Int J Oral Maxillofac Implants 1994;9(2):149-55.