Artigo apresenta terapia aplicada a um implante dentário mal posicionado na região do 46, com diagnóstico clínico e radiográfico de peri-implantite.
AUTORES
Rafaela Nigro
Graduanda em Odontologia – Fousp.
Orcid: 0000-0001-9881-6224.
Marília C. Cavalcanti
Especialista em Periodontia – FOP – Unicamp; Mestra e doutora em Periodontia – Fousp.
Orcid: 0000-0001-5861-9760.
Nayara T. De Lucena
Especialista em Implantodontia – Fundecto/Fousp.
Orcid: 0000-0002-7053-5620.
Giuseppe Alexandre Romito
Professor doutor titular da disciplina de Periodontia – Fousp.
Orcid: 0000-0001-5669-912X.
Claudio Mendes Pannuti
Professor doutor da disciplina de Periodontia – Fousp.
Orcid: 0000-0003-4181-3975.
João Batista César Neto
Professor doutor da disciplina de Periodontia– Fousp.
Orcid: 0000-0002-6823-6170.
RESUMO
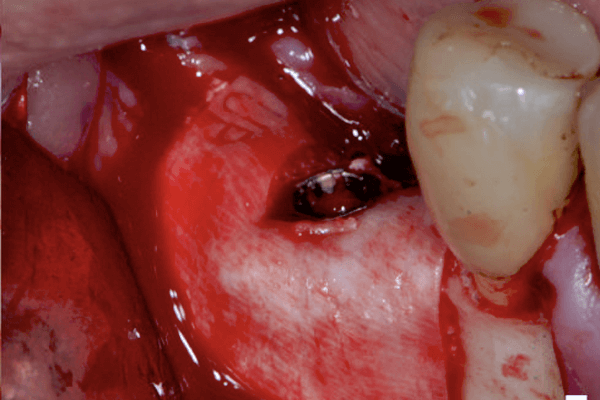
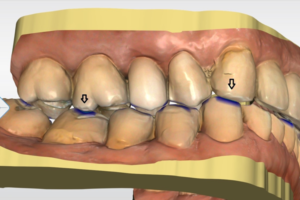
Este relato de caso teve como objetivo apresentar uma terapia aplicada a um implante dentário mal posicionado na região do 46, com diagnóstico clínico e radiográfico de peri-implantite. Para o planejamento do caso, foi levada em consideração a vontade do paciente em manter o implante. Inicialmente, realizou-se drenagem do abscesso e raspagem da região para controle da infecção aguda e desconforto doloroso. Posteriormente, a intervenção terapêutica foi a descontaminação com pontas ultrassônicas convencionais, implantoplastia nas faces livres do implante com pontas diamantadas em alta rotação e terapia cirúrgica regenerativa do defeito ósseo peri-implantar, com substituto ósseo bovino desproteinizado e membrana de colágeno. Após a fase cirúrgica do tratamento, o paciente continua no programa de controle periodontal e peri-implantar a cada quatro meses. Após dois anos de acompanhamento, o sítio do implante apresentou-se saudável, sendo possível devolver função e estética para o paciente. Pôde-se concluir que a terapia aplicada para tratamento da peri-implantite neste caso clínico foi eficaz, resultando em tecidos peri-implantares saudáveis ao longo do tempo.
Palavras-chave – Implante dentário; Peri-implantite; Implantoplastia; Regeneração óssea guiada.
ABSTRACT
Peri-implantitis is the inflammation of the peri-implant mucosa and the progressive loss of supporting bone. Despite being a prevalent clinical condition, there is no consensus in literature on an ideal treatment protocol. This case report aims to present a therapy applied to a buccally positioned dental implant, in the region of 46, with clinical and radiographic diagnosis of peri-implantitis. In planning phase, the patient’s willingness to maintain the implant was taken into account. Initially, the abscess was drained, and the region was debrided to control the acute infection and pain. Subsequently, the therapeutic intervention elected was decontamination with conventional ultrasonic scaler tips, implantoplasty on the exposed surface of the implant with high speed diamond burrs, and then a regenerative surgical therapy of the peri-implant bone defect was performed with a deproteinized bovine bone substitute and collagen membrane. After the surgical phase, the patient was enrolled on a periodontal and peri-implant maintenance program every 4 months. After 2 years of follow-up, the implant site was healthy and it was possible to restore function and aesthetic to the patient. Therefore, it can be concluded that the therapy for the peri-implantitis in this case was effective, resulted in healthy tissues over time.
Key words – Dental implant; Peri-implantitis; Implantoplasty; Guided bone regeneration.
Recebido em abr/2020
Aprovado em jun/2020
Referências
- Hämmerle CFH, Tarnow D. The etiology of hard- and soft-tissue deficiencies at dental implants: a narrative review. J Periodontol 2018;89(suppl.1):291-303.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol 2018;89(suppl.1):267-90.
- Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol 2008;35(8 suppl.):286-91.
- Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 2018;89(suppl.1):313-8.
- Sapata VM, de Souza AB, Sukekava F, Villar CC, César Neto JB. Multidisciplinary treatment for peri-implantitis: a 24-month follow-up case report. Clin Adv Periodontics 2016;6(2):76-82.
- Taiete T, Monteiro MF, Palma MAG, Ruiz KGS, Casarin RCV, Nociti Jr. FH. Regeneração óssea guiada no tratamento de peri-implantite: dois anos de acompanhamento clínico. ImplantNewsPerio 2016;1(8):1607-16.
- Duarte CA, Araujo IMP, Castro MVM, Sarabia MDCM. Vestibuloplastia peri-implantar associada à regeneração tecidual guiada no tratamento da peri-implantite. ImplantNewsPerio 2017;2(4):739-45.
- Lindhe J, Meyle J, Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol 2008;35(8 suppl.):282-5.
- Heitz-Mayfield LJ, Needleman I, Savi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants 2014;29(suppl.):346-50.
- Schwarz F, Sahm N, Iglhaut G, Becker J. Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Priodontol 2011;38(3):276-84.
- Katafuchi M, Weinstein BF, Leroux BG, Chen YW, Daubert DM. Restoration contour is a risk indicator for peri-implantitis: a cross-sectional radiographic analysis. J Clin Periodontol 2018;45(2):225-32.
- Schwarz F, Sahm N, Schwarz K, Becker J. Impact of defect configuration on the clinical outcome following surgical regenerative therapy of peri-implantitis. J Clin Periodontol 2010;37(5):449-55.
- Mir-Mari J, Wui H, Jung RE, Hämmerle CH, Benic GI. Influence of blinded wound closure on the volume stability of different GBR materials: an in vitro cone-beam computed tomographic examination. Clin Oral Implants Res 2016;27(2):258-65.
- Louropoulou A, Slot DE, Van der Weijden F. The effects of mechanical instruments on contaminated titanium dental implant surfaces: a systematic review. Clin Oral Implants Res 2014;25(10):1149-60.
- Valderrama P, Blansett JA, Gonzalez MG, Cantu MG, Wilson TG. Detoxification of implant surfaces affected by peri-implant disease: an overview of non-surgical methods. Open Dent J 2014;16(8):77-84.
- Sato S, Kishida M, Ito K. The comparative effect of ultrasonic scalers on titanium surfaces: an in vitro study. J Periodontol 2004;75(9):1269-73.
- Schwarz F, John G, Schmucker A, Sahm N, Becker J. Combined surgical therapy of advanced peri-implantitis evaluating two methods of surface decontamination: a 7-year follow-up observation. J Clin Periodontol 2017;44(3):337-42.
- Stavropoulos A, Bertl K, Eren S, Gotfredsen K. Mechanical and biological complications after implantoplasty – a systematic review. Clin Oral Implants Res 2019;30(9):833-48.
- Chan HL, Oh WS, Ong HS, Fu JH, Steigmann M, Sierra Alta M. Impact of implantoplasty on strength of the implant-abutment complex. Int J Oral Maxillofac Implants 2013;28(6):1530-5.
- de Souza Júnior JM, Oliveira de Souza JG, Pereira Neto AL, Iaculli F, Piattelli F, Bianchini MA. Analysis of effectiveness of different rotational instruments in implantoplasty: an in vitro study. Implant Dent 2016;25(3):341-7.
- Wessing B, Lettner S, Zechner W. Guided bone regeneration with collagen membranes and particulate graft materials: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 2018;33(1):87-100.
- Suárez-López Del Amo F, Yu S-H, Wang H-L. Non-surgical therapy for peri-implant diseases: a systematic review. J Oral Maxillofac Res 2016;7(3):e13.
- Chambrone L, Wang HL, Romanos GE. Antimicrobial photodynamic therapy for the treatment of periodontitis and peri-implantitis: an American Academy of Periodontology best evidence review. J Periodontol 2018;89(7):783-803.
- Keeve PL, Koo KT, Ramanauskaite A, Romanos G, Schwarz F, Sculean A et al. Surgical treatment of periimplantitis with non-augmentative techniques. Implant Dent 2019;28(2):177-86.
- Rösing CK, Fiorini T, Haas AN, Muniz FWMG, Oppermann RV, Susin C. The impact of maintenance on peri-implant health. Braz Oral Res 2019;30(suppl.1):e074.