RESUMO
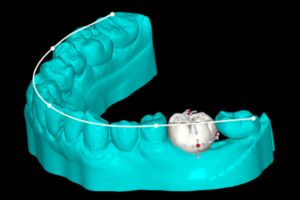
Este artigo descreveu o tratamento de um caso de fenestração radicular decorrente de terapia endodôntica na região do dente 33. Foi realizada exodontia atraumática preservando a faixa óssea coronal e apical ao defeito. Prosseguiu-se com a instalação de implante, além de regeneração tecidual e óssea guiada com a utilização de membrana colágena em formato T, inserida através de tunelização e com técnica de sutura própria. A resolução clínica deste caso deu-se, entre outros fatores, através da técnica de escolha para inserção e sutura da membrana colágena, que permitiu sua fixação à mucosa e a cobertura da fenestração sem a elevação de retalho, favorecendo a regeneração tecidual. O fenômeno chamado creeping attachment, embora imprevisível, pode ter contribuído para o desfecho favorável ao longo do tempo do presente caso. A técnica para inserção e sutura da membrana colágena com tunelização escolhida foi favorável para o fechamento da lesão de fenestração. No entanto, mais estudos clínicos similares são necessários para ratificar a reprodutibilidade e eficácia da técnica relatada.
Palavras-chave – Regeneração tecidual guiada; Implantes dentários; Técnicas de sutura; Fenestração gengival.
ABSTRACT
This paper describes the treatment of a case of root fenestration resulting from endodontic treatment in the region of tooth 33. After atraumatic tooth extraction has been performed, the coronal and apical bone regions to the defect were preserved. This was followed by the installation of a dental implant, in addition to guided tissue and bone regeneration using a T-shaped collagen membrane, inserted through tunneling and using a specific suturing technique. The clinical resolution of this case occurred, among other factors, through the chosen technique for insertion and suturing of the collagenous membrane, which allowed its fixation to the mucosa and coverage of the fenestration without flap elevation, favoring tissue regeneration. The phenomenon of creeping attachment, although unpredictable, may have contributed to the favorable outcome over time in the present case. The technique for insertion and suture of the collagen membrane with tunneling chosen was favorable for closing the fenestration lesion. However, more similar clinical studies are needed to confirm the reproducibility and efficacy of the reported technique.
Key words – Guided tissue regeneration; Dental implants; Suture techniques; Root fenestration.
Referências
- Pendor S, Baliga V, Muthukumaraswamy A, Dhadse PV, Ganji KK, Thakare K. Coverage of gingival fenestration using modified pouch and tunnel technique: a novel approach. Case Rep Dent 2013;2013:902585.
- Edel A. Alveolar bone fenestrations and dehiscences in dry Bedouin jaws. J Clin Periodontol 1981;8(6):491-9.
- Patel PV, Kumar N, Durrani F. Microsurgical aesthetic treatment of gingival fenestration by a coronally repositioned partial thickness graft: a case report. J Clin Diagn Res 2013;7(11):2649-50.
- Santos-Pinto LA, Seale NS, Reddy AK, Cordeiro RC. Fenestration gingival defect in erupting permanent mandibular incisors: a case report. Quintessence Int 1998;29(4):239-42.
- Rajula MPB, Varatharajan K, Mani R, Krishnakumar S. Gingival fenestration management: a rarefied case entity and literature review. J Pharm Bioallied Sci 2020;12(suppl.1):648-51.
- Yang ZP. Treatment of labial fenestration of maxillary central incisor. Endod Dent Traumatol 1996;12(2):104-8.
- Goldman HM, Cohen DW. Periodontal therapy (3rd). St. Louis: The C. V. Mosby Company. p.1964-560.
- Matter J, Cimasoni G. Creeping attachment after free gingival grafts. J Periodontol 1976;47(10):574-9.
- Parra C, Capri D. Peri-implant mucosal creeping: two case reports. Int J Periodontics Restorative Dent 2018;38(2):227-33.
- Pereira Neto AR, Passoni BB, de Souza Jr. JM, de Souza JG, Benfatti CA, Magini RS et al. Creeping attachment involving dental implants: two case reports with a two-year follow-up from an ongoing clinical study. Case Rep Dent 2014:2014:756908.
- Agudio G, Nieri M, Rotundo R, Cortellini P, Pini Prato G. Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. J Periodontol 2008;79(4):587-94.
- Schierano G, Ramieri G, Cortese M, Aimetti M, Preti G. Organization of the connective tissue barrier around long-term loaded implant abutments in man. Clin Oral Implants Res 2002;13(5):460-4.
- Buser D, Hoffmann B, Bernard JP, Lussi A, Mettler D, Schenk RK. Evaluation of filling materials in membrane – protected bone defects. A comparative histomorphometric study in the mandible of miniature pigs. Clin Oral Implants Res 1998;9(3):137-50.
- Dimitriou R, Mataliotakis GI, Calori GM, Giannoudis PV. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: current experimental and clinical evidence. BMC Med 2012:10:81.
- Dubey N, Ferreira JA, Malda J, Bhaduri SB, Bottino MC. Extracellular matrix/amorphous magnesium phosphate bioink for 3d bioprinting of craniomaxillofacial bone tissue. ACS Appl Mater Interfaces 2020;12(21):23752-63.
- Zhuang Y, Lin K, Yu H. Advance of nano-composite electrospun fibers in periodontal regeneration. Front Chem 2019;7:495.
- Hur Y, Tsukiyama T, Yoon TH, Griffin T. Double flap incision design for guided bone regeneration: a novel technique and clinical considerations. J Periodontol 2010;81(6):945-52.
- Ogata Y, Griffin TJ, Ko AC, Hur Y. Comparison of double-flap incision to periosteal releasing incision for flap advancement: a prospective clinical trial. Int J Oral Maxillofac Implants 2013;28(2):597-604.
- Hasuike A, Ujiie H, Senoo M, Furuhata M, Kishida M, Akutagawa H et al. Pedicle periosteum as a barrier for guided bone regeneration in the rabbit frontal bone. In Vivo 2019;33(3):717-22.
- Hämmerle CH, Giannobile WV, Working Group 1 of the European Workshop on Periodontology. Biology of soft tissue wound healing and regeneration- consensus report of Group 1 of the 10th European Workshop on Periodontology. J Clin Periodontol 2014;41(suppl.15):S1-5.
- Santos A, Goumenos G, Pascual A, Nart J. Creeping attachment after 10 years of treatment of a gingival recession with acellular dermal matrix: a case report. Quintessence Int 2011;42(2):121-6.
- Matter J. Free gingival grafts for the treatment of gingival recession. A review of some techniques. J Clin Periodontol 1982;9(2):103-14.
- Borghetti A, Gardella JP. Thick gingival autograft for the coverage of gingival recession: a clinical evaluation. Int J Periodontics Restorative Dent 1990;10(3):216-29.
- Bell LA, Valluzzo TA, Garnick JJ, Pennel BM. The presence of “creeping attachment” in human gingiva. J Periodontol 1978;49(10):513-7.
- Parra C, Capri D. Peri-implant mucosal creeping: two case reports. Int J Periodontics Restorative Dent 2018;38(2):227-33.
- Wan W, Zhong H, Wang J. Creeping attachment: a literature review. J Esthet Restor Dent 2020;32(8):776-82.