Artigo avalia a alteração dimensional do osso mineral bovino desproteinizado no procedimento de levantamento de seio maxilar.
RESUMO
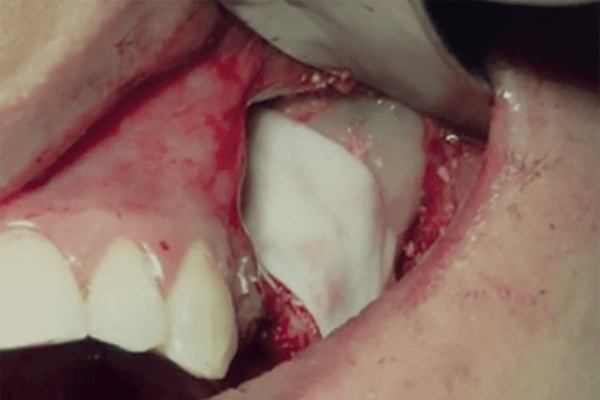
Objetivo: avaliar a alteração dimensional do osso mineral bovino desproteinizado no procedimento de levantamento de seio maxilar após oito meses. Material e métodos: 12 pacientes, com altura óssea remanescente menor ou igual a 5 mm, receberam levantamento bilateral dos seios maxilares. No grupo-controle (GC), foi utilizado apenas DBBM (Bio-Oss); no grupo experimental (GE), utilizou-se DBBM associado a 0,3 cc de EMD (Emdogain) – DBBM+EMD. Os grupos GC e GE foram divididos em 50% no seio direito e 50% no seio esquerdo. Os pacientes foram submetidos à tomografi a computadorizada de feixe cônico (TCFC) imediatamente após a cirurgia (T1) e após oito meses (T2). As imagens de T1 e T2 foram importadas para o cálculo da área do enxerto. Observou-se uma redução média percentual da área do enxerto de 15,31% no GC e de 11,21% no GE, sem diferença estatisticamente signifi cativa. Conclusão: em curto prazo, associar DBBM ou não ao EMD no levantamento de seio maxilar demonstra pouco impacto sob o ponto de vista tomográfi co. Entretanto, mais investigações em longo prazo são necessárias.
Palavras-chave – Levantamento do assoalho do seio maxilar; Xenoenxertos; Derivado da matriz do esmalte.
ABSTRACT
Objective: to evaluate the dimensional change of deproteinized bovine mineral bone in the maxillary sinus lift procedure aft er 8 months. Material and methods: twelve patients, with remaining bone height less than or equal to 5 mm, received bilateral maxillary sinus lift s. In the control group (CG), only DBBM (Bio-Oss) was used and in the experimental group (EG) DBBM associated with 0.3 cc of EMD (Emdogain) – DBBM+EMD was used. The CG and EG groups were divided into 50% in the right maxillary sinus and 50% in the left . Patients underwent cone beam computed tomography (CBCT) immediately aft er surgery (T1) and aft er eight months (T2). T1 and T2 images were imported to calculate the graft area. The percentage mean reduction observed in graft area was 15.31% in the CG and 11.21% in the EG, with no statistically signifi cant diff erence. Conclusion: in the short-term, associating DBBM or not with EMD in the maxillary sinus lift shows little impact from the tomographic point of view. However, more long-term studies are needed.
Key words – Sinus fl oor augmentation; Xenograft ; Enamel matrix derivative.
Referências
- Boyne P, James RA. Grafting of the maxillary sinus floor with autogenous marrows and bone. J Oral Surg 1980;38(8):613-6.
- Tatum Jr. H. Maxillary and sinus implant reconstructions. Dent Clin North Am 1986;30(2):207-28.
- Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol 1987;4(2):49-58.
- Artzi Z, Kolovsky A, Nemcovsky CE, Weinreb M. The amount of newly formed bone in sinus grafting procedures depends on tissue depth as well as the type and residual amount of the grafted material. J Clin Periodontol 2005;32(2):193-9.
- Froum SJ, Wallace SS, Cho SC, Elian N, Tarnow DP. Histomorphometric comparison of a biphasic bone ceramic to anorganic bovine bone for sinus augmentation: 6- to 8- month post chirurgical assessment of vital bone formation. A pilot study. Int J Periodontics Restorative Dent 2008;28(3):273-81.
- Jensen T, Schou S, Svendsen PA, Forman JL, Gundersen HJ, Terheyden H et al. Volumetric changes of the graft after maxillary sinus floor augmentation with Bio-Oss® and autogenous bone in different ratios: a radiographic study in minipigs. Clin Oral Implants Res 2012;23(8):902-10.
- Liu Y, Wang J, Chen F, Feng Y, Xie C, Li D. A reduced healing protocol for sinus floor elevation in a staged approach with deproteinized bovine bone mineral alone: a randomized controlled clinical trial of a 5-month healing in comparison to the 8-month healing. Clin Implant Dent Relat Res 2020;22(3):281-91.
- Bartlett CS, Rapuano BE, Lorich DG, Wu T, Anderson RC, Tomin E et al. Early changes in prostaglandins precede bone formation in a rabbit model of heterotopic ossification. Bone 2006;38(3):322-32.
- Margolis RN, Wimalawansa SJ. Novel targets and therapeutics for bone loss. Ann N Y Acad Sci 2006;1068:402-9.
- Lyngstadaas SP, Wohlfahrt JC, Brookes SJ, Paine ML, Snead ML, Reseland JE. Enamel matrix proteins; old molecules for new applications. Orthod Craniofac Res 2009;12(3):243-53.
- Froum S, Lemler J, Horowitz R, Davidson B. The use of enamel matrix derivative in the treatment of periodontal osseous defects: a clinical decision tree based on biologic principles of regeneration. Int J Periodontics Restorative Dent 2001;21(5):437-49.
- Tonetti MS, Lang NP, Cortellini P, Suvan JE, Adriaens P, Dubravec D et al. Enamel matrix proteins in the regenerative therapy of deep intrabony defects. J Clin Periodontol 2002;29(4):317-25.
- Meyle J, Gonzales JR, Bödeker RH, Hoffmann T, Richter S, Heinz B et al. A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part II: secondary outcomes. J Periodontol 2004;75(9):1188-95.
- Sanz M, Tonetti MS, Zabalegui I, Sicilia A, Blanco J, Rebelo H et al. Treatment of intrabony defects with enamel matrix proteins or barrier membranes: results from a multicenter practice-based clinical trial. J Periodontol 2004;75(5):726-33.
- Simmer JP, Fincham AG. Molecular mechanisms of dental enamel formation. Crit Rev Oral Biol Med 1995;6(2):84-108.
- Froum SJ, Wallace SS, Elian N, Cho SC, Tarnow DP. Comparison of mineralized cancellous bone allograft (Puros) and anorganic bovine bone matrix (Bio-Oss) for sinus augmentation: histomorphometry at 26 to 32 weeks after grafting. Int J Periodontics Restorative Dent 2006;26(6):543-51.
- Chackartchi T, Iezzi G, Goldstein M, Klinger A, Soskolne A, Piattelli A et al. Sinus floor augmentation using large (1-2 mm) or small (0.25-1 mm) bovine bone mineral particles: a prospective, intra-individual controlled clinical, micro-computerized tomography and histomorphometric study. Clin Oral Implants Res 2011;22(5):473-80.
- Testori T, Wallace SS, Trisi P, Capelli M, Zuffetti F, Del Fabbro M. Effect of xenograft (ABBM) particle size on vital bone formation following maxillary sinus augmentation: a multicenter, randomized, controlled, clinical histomorphometric trial. Int J Periodontics Restorative Dent 2013;33(4):467-75.
- Jensen SS, Aaboe M, Janner SF, Saulacic N, Bornstein MM, Bosshardt DD et al. Influence of particle size of deproteinized bovine bone mineral on new bone formation and implant stability after simultaneous sinus floor elevation: a histomorphometric study in minipigs. Clin Implant Dent Relat Res 2015;17(2):274-85.
- Piattelli M, Favero GA, Scarano A, Orsini G, Piattelli A. Bone reactions to anorganic bovine bone (Bio-Oss) used in sinus augmentation procedures: a histologic long-term report of 20 cases in humans. Int J Oral Maxillofac Implants 1999;14(6):835-40.
- Maiorana C, Sigurtà D, Mirandola A, Garlini G, Santoro F. Bone resorption around dental implants placed in grafted sinuses: clinical and radiologic follow-up after up to 4 years. Int J Oral Maxillofac Implants 2005;20(2):261-6.
- Pebé PJ, Ramos-Yanuzzi A, Beovide AV, Borgia G, Ravecca T. A randomized clinical trial comparing two particle sizes in lateral window sinus lift with deproteinized bovine bone mineral: clinical and histological results. Odontoestomatol 2017;19:57-67.
- de Souza SLS, Messora MR, Gabarra Junior JAB, Mantovani RV, da Costa LFA, Martins SHL et al. Absorção do osso bovino inorgânico utilizado em levantamento do seio maxilar. Caso clínico com avaliações microtomográfica e histomorfométrica após 12 e 20 meses. ImplantNews 2014;11(6a):69-76.
- Jensen SS, Broggini N, Hjørting-Hansen E, Schenk R, Buser D. Bone healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clin Oral Implants Res 2006;17(3):237-43.
- Shimizu-Ishiura M, Tanaka S, Lee WS, Debari K, Sasaki T. Effects of enamel matrix derivative to titanium implantation in rat femurs. J Biomed Mater Res 2002;60(2):269-76.
- Reichert C, Al-Nawas B, Smeets R, Kasaj A, Götz W, Klein MO. In vitro proliferation of human osteogenic cells in presence of different commercial bone substitute materials combined with enamel matrix derivatives. Head Face Med 2009;5:23.
- Miron RJ, Oates CJ, Molenberg A, Dard M, Hamilton DW. The effect of enamel matrix proteins on the spreading, proliferation and differentiation of osteoblasts cultured on titanium surfaces. Biomaterials 2010;31(3):449-60.
- Potijanyakul P, Sattayasansakul W, Pongpanich S, Leepong N, Kintarak S. Effects of enamel matrix derivative on bioactive glass in rat calvarium defects. J Oral Implantol 2010;36(3):195-204.
- Casati MZ, Sallum EA, Nociti Jr. FH, Caffesse RG, Sallum AW. Enamel matrix derivative and bone healing after guided bone regeneration in dehiscence-type defects around implants. A histomorphometric study in dogs. J Periodontol 2002;73(7):789-96.
- Vincent-Bugnas S, Charbit Y, Charbit M, Dard M, Pippenger B. Maxillary sinus floor elevation surgery with biooss mixed with enamel matrix derivative: a human randomized controlled clinical and histologic study. J Oral Implantol 2020;46(5):507-13.
- Murai M, Sato S, Koshi R, Yokoyama K, Ikeda K, Narukawa M et al. Effects of the enamel matrix derivative and beta-tricalcium phosphate on bone augmentation within a titanium cap in rabbit calvarium. J Oral Sci 2005;47(4):209-17.