Erupção passiva: trabalho apresenta caso clínico de uma paciente que se queixava de “dentes curtos” e diferença de tamanho.
AUTORES
Rafael Sponchiado Cavallieri
Mestrando do programa de Ciências Odontológicas, disciplina de Periodontia – FOB-USP; Especialista em Periodontia – HRAC-USP.
Orcid: 0000-0003-3975-6211.
Caique Andrade Santos
Mestrando do programa de Ciências Odontológicas, disciplina de Periodontia – FOB-USP.
Orcid: 0000-0001-5646-3424.
Sebastião Luiz Aguiar Greghi
Professor doutor titular da disciplina de Periodontia – FOB-USP.
Orcid: 0000-0003-2530-3705.
Adriana Campos Passanezi Sant’Ana
Professora doutora associada da disciplina de Periodontia – FOB-USP.
Orcid: 0000-0001-5640-9292.
Carla Andreotti Damante
Professora doutora associada da disciplina de Periodontia – FOB-USP.
Orcid: 0000-0002-6782-8596.
Mariana Schutzer Ragghianti Zangrando
Professora doutora assistente da disciplina de Periodontia – FOB-USP.
Orcid: 0000-0003-0286-7575.
RESUMO
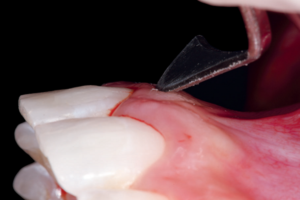
Entre as desarmonias do sorriso, o excesso de exposição gengival pode ser associado a diferentes causas, como o excesso vertical de maxila, extrusão dentoalveolar, lábio superior curto, hipermobilidade labial, erupção passiva e/ou ativa alteradas, ou uma combinação desses fatores. O objetivo deste trabalho foi apresentar o caso clínico de uma paciente com 22 anos que se queixava dos “dentes curtos” de 14 a 24 e da diferença de tamanho entre os elementos 11 e 21. Para diagnóstico e planejamento, foi utilizada tomografia computadorizada de feixe cônico (TCFC), diagnosticando assim erupção passiva alterada (EPA) em todos os dentes e erupção ativa alterada (EAA) nos caninos e pré-molares. Na técnica cirúrgica, foi realizada incisão em bisel interno (45°) e discreta frenectomia labial, retalho total para a osteotomia e osteoplastia com pontas diamantadas, e sutura com fio de nylon 5-0 em colchoeiro vertical. No pós-operatório imediato e durante mais três sessões com intervalo de 48 horas, foi realizada fotobiomodulação com laser vermelho para auxiliar na cicatrização dos tecidos moles. As suturas foram removidas em 14 dias e a paciente acompanhada até o momento (90 dias de pós-operatório). A EPA e EAA não são consideradas patologias, mas variações da normalidade, o correto diagnóstico, conhecimento dos tecidos de inserção supracrestal, princípios periodontais de preservação de mucosa ceratinizada e identificação de fenótipo gengival garantem excelência em resultados a longo prazo. Além disso, ferramentas digitais, como a TCFC, podem auxiliar no planejamento e na previsibilidade do tratamento.
Palavras-chave – Periodontia; Aumento da coroa clínica; Terapia a laser.
ABSTRACT
Among smile disharmonies, excessive gingival exposure can be associated with different causes such as vertical maxillary excess, dentoalveolar extrusion, short upper lip, labial hypermobility, altered passive and active eruption, or a combination of these factors. The aim of this study is to present the clinical case of a 22-year-old patient who complained of “short teeth” from 14 to 24 and the difference between the sizes of 11 and 21. For diagnosis and planning, CBCT was performed, thus diagnosing altered passive eruption (APE) in all teeth and active altered eruption (AAE) at canines and premolars. Regarding the surgical techniques, a bevelled internal incision was placed at 45 degrees with a discrete lip frenectomy, raising a full tissue flap for osteotomy and osteoplasty with diamond burs; then, a vertical mattress 5-0 nylon suture was placed to close the surgical area. After, red laser photobiomodulation was used immediately after and for three sessions (48h intervals each) to help in the soft tissue healing. The sutures were removed 14 days later and the patient followed up to 90 days. APE and AAE are not considered pathologies, but variations from normality, correct diagnosis, knowledge of supracrestal attachment tissues, periodontal principles of preservation of keratinized mucosa and identification of gingival phenotype ensure excellence in long-term results. In addition, digital tools such as CT can help with treatment planning and predictability.
Key words – Periodontics; Crown lengthening; Laser therapy.
Referências
- Priest G, Priest J. Promoting esthetic procedures in the prosthodontic practice. J Prosthodont 2004;13(2):111-7.
- Levine RA, McGuire M. The diagnosis and treatment of the gummy smile. Compend Contin Educ Dent 1997;18(8):757-62.
- Goldman HD, Cohen D. Periodontal therapy (4a). St. Louis: The CV Mosby Company, 1968.
- Amsterdam MA. Form and function of the masticatory system. Philadelphia: University of Pennsylvania, 1991.
- Zangrando MSR, Veronesi GF, Cardoso MV, Michel RC, Damante CA, Sant’Ana ACP et al. Altered active and passive eruption: a modified classification. Clin Adv Periodontics 2017;7(1):51-6.
- Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan 1977;70(3):24-8.
- Cayana EG, Greggianin BF, Angst PD, Gomes SC, Oppermann RV. Measuring periodontal biologic distances: transperiodontal vs transurgical probing. Acta Odontol Scand 2013;71(6):1632-5.
- Zanatta FB, Giacomelli BR, Dotto PP, Fontanella VR, Rosing CK. Comparison of different methods involved in the planning of clinical crown lengthening surgery. Braz Oral Res 2010;24(4):443-8.
- Januário AL, Barriviera M, Duarte WR. Soft tissue cone-beam computed tomography: a novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent 2008;20(6):366-73.
- Olsson M, Lindhe J, Marinello CP. On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol 1993;20(8):570-7.
- Nart J, Carrió N, Valles C, Solís-Moreno C, Nart M, Reñé R et al. Prevalence of altered passive eruption in orthodontically treated and untreated patients. J Periodontol 2014;85(11):e348-53.
- Garber DA, Maurice AS. The aesthetic smile: diagnosis and treatment. Periodontol 2000 1996;11(1):18-28.
- Khadra M, Kasem N, Lyngstadaas SP, Haanaes HR, Mustafa K. Laser therapy accelerates initial attachment and subsequent behaviour of human oral fibroblastos cultured on titanium implant material. A scanning electron microscope and histomorphometric analysis. Clin Oral Implants Res 2005;16(2):168-75.
- Ozturan S, Durukan SA, Ozcelik O, Seydaoglu G, Haytac MC. Coronally advanced flap adjunct with low intensity laser therapy: a randomized controlled clinical pilot study. J Clin Periodontol 2011;38(11):1055-62.
- Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol 2003;74(4):557-62.
- Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent 2010;30(3):237-43.
- Joly JC, de Carvalho PF, da Silva RC. Reconstrução tecidual estética: procedimentos plásticos e regenerativos periodontais e peri-implantares (1a). Porto Alegre: Artes Médicas, 2009.
- Metin R, Tatli U, Evlice B. Effects of low-level laser therapy on soft and hard tissue healing after endodontic surgery. Lasers Med Sci 2018;33(8):1699-706.
- Sella VRG, Bomfim FRC, Machado PCD, Morsoleto MJMS, Chohfi M, Plapler H. Effect of low-level laser therapy on bone repair: a randomized controlled experimental study. Lasers Med Sci 2015;30(3):1061-8.
- Korany NS, Mehanni SS, Hakam HM, El-Maghraby EMF. Evaluation of socket healing in irradiated rats after diode laser exposure (histological and morphometric studies). Arch Oral Biol 2012;57(7):884-91.
- Abd-Elaal AZ, El-Mekawii HA, Saafan AM, El Gawad LA, El-Hawary YM, Abdelrazik MA. Evaluation of the effect of low-level diode laser therapy applied during the bone consolidation period following mandibular distraction osteogenesis in the human. Int J Oral Maxillofac Surg 2015;44(8):989-97.