RESUMO
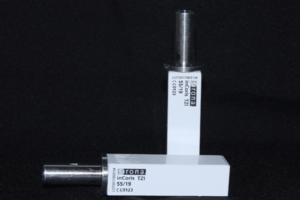
Atualmente, encontram-se disponíveis componentes protéticos compatíveis aos componentes originais, buscando diminuir os custos das restaurações implantossuportadas. Ainda restam dúvidas quanto à qualidade desses componentes em relação aos originais. Este trabalho avaliou a adaptação de componentes protéticos originais e multiplataformas com o auxílio de microtomografia computadorizada. Os implantes (NobelReplace Conical Connection) foram divididos em quatro grupos (n=1) – G1: componente original (Pilar Universal Base CC NP 1,5 mm); G2: componente EFF (Pilar Universal Base NP cinta 1,5 mm); G3: componente Conexão (TiBase Standard Morse Indexado NP 1,5 mm x 4,5 mm); e G4: componente Dérig (Interface NP 1,5 mm x 4,5 mm). O componente de cada grupo foi fixado com torque de 25 Ncm, de acordo com as instruções do fabricante. Foram definidas quatro regiões de interesse nas imagens para avaliar a adaptação entre os componentes. Os resultados foram então comparados estatisticamente (p=0,05) – InStat, GraphPad Software. Nas regiões 1 e 2, o grupo G3 apresentou a maior interface de conexão entre as superfícies do implante e componente protético (p < 0,05). Contudo, todos os grupos apresentaram valores elevados nessas regiões. Já nas regiões 3 e 4, localizadas na interface formada entre o parafuso do pilar protético e o próprio pilar, os grupos G1 e G2 apresentaram os maiores valores de contato entre as interfaces, em comparação com os outros grupos do estudo (p < 0,05). A adaptação na interface cônica da conexão protética foi adequada para todos os grupos avaliados no estudo. Os grupos G3 e G4 apresentaram menor superfície de contato na interface formada entre o parafuso do componente e o componente protético.
Palavras-chave – Implantes dentários; Pilares protéticos; Adaptação interna; Microtomografia computadorizada.
ABSTRACT
The use of implant-supported restorations increased the availability of prosthetic abutments for multiple platforms aiming to reduce rehabilitation costs. The quality of multiplatform prosthetic abutments remains unclear. This study used computerized microtomography (micro-CT) to analyze the misfit at the implant-abutment interface of original and multiplatform abutments. The implants (NobelReplace Conical Connection) were divided in 4 groups (n=1) – G1: original abutment (Pilar Universal Base CC NP 1.5 mm), G2: EFF abutment (Pilar Universal Base NP cinta 1.5 mm); G3: Conexão abutment (TiBase Standard Morse Indexado NP 1.5 x 4.5 mm); and G4: Dérig abutment (Interface NP 1.5 x 4.5 mm). Each prosthetic abutment was screwed to the implant with a 25 Ncm torque load, according to instructions from the manufacturer. Four regions of interest were defined in the micro-CT images to evaluate misfit. The results were statistically compared with the aid of specialized software (p=0.05) – InStat, GraphPad Software. Group G3 had the highest contact interface between implant and abutment on regions of interest 1 and 2 (p < 0.05). However, all groups in the study showed high interface contact levels at the same regions of interest. Groups G1 and G2 showed the highest contact interfaces on regions of interest 3 and 4, located at the prosthetic abutment screw and the prosthetic abutment itself (p < 0.05). The fit of the abutments and implants at the tapered interface was adequate for all groups in the study. However, groups G3 and G4 showed a limited contact interface between the abutment screw and the abutment itself.
Key words – Dental implants; Prosthetic abutments; Internal fit; Computerized microtomography.
Referências
- Honorio Tonin BS, He Y, Ye N, Chew HP, Fok A. Effects of tightening torque on screw stress and formation of implant-abutment microgaps: a finite element analysis. J Prosthet Dent 2022;127(6):882-9.
- Sammour SR, Maamoun El-Sheikh M, Aly El-Gendy A. Effect of implant abutment connection designs, and implant diameters on screw loosening before and after cyclic loading: in-vitro study. Dent Mater 2019;35(11):e265-e71.
- Schmitt CM, Nogueira-Filho G, Tenenbaum HC, Lai JY, Brito C, Doring H et al. Performance of conical abutment (Morse Taper) connection implants: a systematic review. J Biomed Mater Res A 2014;102(2):552-74.
- Yao KT, Kao HC, Cheng CK, Fang HW, Huang CH, Hsu ML. Mechanical performance of conical implant-abutment connections under different cyclic loading conditions. J Mech Behav Biomed Mater 2019;90:426-32.
- Gupta S, Gupta H, Tandan A. Technical complications of implant-causes and management: a comprehensive review. Natl J Maxillofac Surg 2015;6(1):3-8.
- He Y, Fok A, Aparicio C, Teng W. Contact analysis of gap formation at dental implant-abutment interface under oblique loading: a numerical-experimental study. Clin Implant Dent Relat Res 2019;21(4):741-52.
- Oziunas R, Sakalauskiene J, Jegelevicius D, Januzis G. A comparative biomechanical study of original and compatible titanium bases: evaluation of screw loosening and 3D-crown displacement following cyclic loading analysis. J Adv Prosthodont 2022;14(2):70-7.
- da Cunha TMA, de Araujo RP, da Rocha PV, Amoedo RM. Comparison of fit accuracy between Procera(R) custom abutments and three implant systems. Clin Implant Dent Relat Res 2012;14(6):772-7.
- Cardoso KB, Bergamo ETP, Cruz VM, Ramalho IS, Lino LFO, Bonfante EA. Three-dimensional misfit between Ti-Base abutments and implants evaluated by replica technique. J Appl Oral Sci 2020;28:e20200343.
- Berberi A, Maroun D, Kanj W, Amine EZ, Philippe A. Micromovement evaluation of original and compatible abutments at the implant-abutment interface. J Contemp Dent Pract 2016;17(11):907-13.
- Gao J, Min J, Chen X, Yu P, Tan X, Zhang Q et al. Effects of two fretting damage modes on the dental implant–abutment interface and the generation of metal wear debris: an in vitro study. Fatigue & Fracture of Engineering Materials & Structures 2021;44(3):847-58.
- Berberi A, Tehini G, Rifai K, Bou Nasser Eddine F, Badran B, Akl H. Leakage evaluation of original and compatible implant-abutment connections: in vitro study using Rhodamine B. J Dent Biomech 2014;5:1758736014547143.
- Berberi A, Tehini G, Hjeij B, Aoun G. Evaluation of marginal and internal fit at implant-abutment interface of original and compatible nonoriginal abutments. J Long Term Eff Med Implants 2022;32(3):21-8.