RESUMO
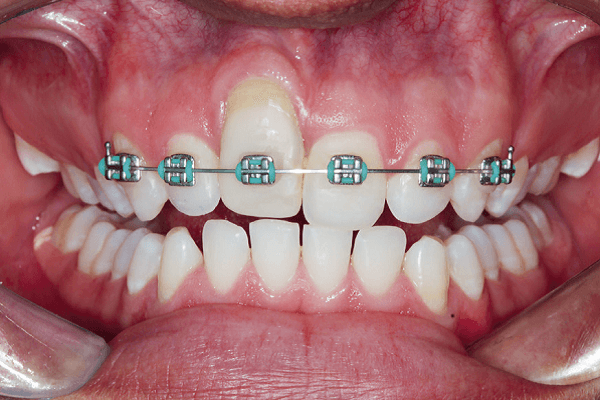
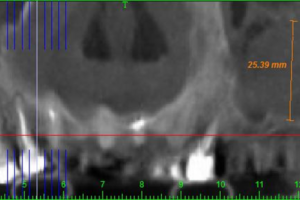
Este relato de caso demonstra uma combinação de estratégias de RTG para alívio do defeito residual na zona estética. Um paciente do sexo masculino havia sofrido um acidente traumático no dente 11 durante a infância, com tratamento endodôntico e reimplantação imediata. Dez anos depois, o desnível entre as margens gengivais era de 10 mm, e uma reabsorção radicular estava presente. Para tentar diminuir a recessão de tecido mole e o contorno ósseo deficiente, uma matriz colágena suína (MucoGraft) foi montada no sentido vertical substituindo a parede vestibular, e o alvéolo de extração foi preenchido com osso bovino inorgânico (Bio-Oss). A coroa dentária natural foi usada como pôntico no aparelho ortodôntico de contenção. Três meses depois, e após um exame por tomografia computadorizada feixe cônico para determinação dos níveis ósseos resultantes, o conjunto implante dentário (3,4 mm x 10 mm)/ pilar (platform-switching) e osso bovino foi colocado no alvéolo cicatrizado, e a coroa natural foi trocada por uma coroa provisória cimentada. Seis meses depois, um enxerto gengival livre foi aplicado. Após o condicionamento do tecido mole, o desnivelamento gengival entre as margens reduziu-se para 2 mm. A restauração definitiva recebeu infraestrutura em zircônia CAD/CAM recoberta por porcelana feldspática. Mesmo que a estratégia combinada tenha se mostrado útil no alívio da situação clínica, estudos longitudinais com amostras maiores são necessários para comprovar sua eficácia.
Palavras-chave – Reabsorção dentária; Extração dentária; Implante dentário; Cirurgia gengival; Matriz de colágeno suíno; Regeneração tecidual.
ABSTRACT
This case report demonstrates a combination of RTG strategies to alleviate a residual defect in the esthetic zone. A male patient had suffered a traumatic accident at the tooth 11 during childhood, with endodontic treatment and immediate replantation. Ten years later, the unbalance between the gingival margins was 10 mm, and a root resorption was detected. In an attempt to reduce the soft tissue recession and poor bone contour, a porcine collagen matrix (MucoGraft) was mounted vertically replacing the labial wall, and the alveolar extraction socket filled with xenogeneic bovine bone (Bio-Oss). The natural dental crown was used as the pontic in the orthodontic device. Three months later and after a cone beam computerized tomography to determine the resulting bone levels, the dental implant (3.4 mm x 10 mm)/abutment (platform-switching) assembly and bovine bone were placed in the healed socket, and the natural crown was replaced by a cemented temporary crown. Six months later, a free gingival graft was applied. After soft tissue conditioning, the unbalance between gingival margins between was reduced to 2 mm. The final restoration received a CAD/CAM zirconia infrastructure veneered with feldspathic porcelain. Even that the combined strategy has proven useful in this clinical situation. Longitudinal studies with larger samples are needed to confirm its effectiveness.
Key words – Tooth resorption; Tooth extraction; Dental implant; Gingival surgery; Porcine collagen matrix; Tissue regeneration.
Referências
- Pommer B, Valkova V, Maheen CU, Fürhauser L, Rausch-Fan X, Seeman R. Scientific interests of 21st century clinical oral implant research: topic trend analysis. Clin Implant Dent Relat Res 2016;18(4):850-6.
- Muglia VA, Novaes Jr. AB. Colocação subcrestal de implantes dentais na reabilitação oral implantossuportada. In: Rossetti PHO, Bonachela WC (eds). Situações Complexas na Implantodontia: soluções clínicas especializadas. São Paulo: VM Cultural, 2013. p.92-123.
- Hamanaka EF, Nogueira LM, Pires WR, Panzarini SR, Poi WR, Sonoda CK. Replantation as treatment for extrusive luxation. Braz Dent J 2015;26(3):308-11.
- Heithersay GS. Life cycles of traumatized teeth: long-term observation from a cohort dental trauma victims. Aust Dent J 2016;61(suppl.1):120-7.
- Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 4 factors related to periodontal ligament healing. Endod Dent Traumatol 1995;11(2):76-89.
- Huynh-Ba G, Pjetursson BE, Sanz M, Cecchinato D, Ferrus J, Lindhe J et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res 2010;21(1):37-42.
- Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall – a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent 2011;31(2):125-31.
- Pinto AVS, Couy KC, Pinto MNS, Paulon P. Tratamento do complexo mucoso alveolar imediato à extração dental. In: Rossetti PHO, Bonachela WC (eds). 50 Anos de Osseointegração: reflexões e perspectivas. São Paulo: VM Cultural, 2015. 200-65.
- Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M. Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 2009;36(10):868-76.
- McGuire MK, Scheyer T. Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 2010;81(8):1108-17.
- Nevins M, Levins ML, Kim SW, Schupbach P, Kim DM. The use of Mucograft collagen matrix to augment the zone of keratinized tissue around teeth: a pilot study. Int J Periodontics Restorative Dent 2011;31(4):367-73.
- Rotundo R, Pini-Prato G. Use of a new collagen matrix (Mucograft) for the treatment of multiple gingival recessions: case reports. Int J Periodontics Restorative Dent 2012;32(4):413-9.
- Reino DM, Maia LP, Fernandes PF, Novaes Jr. AB. Tratamento de retração gengival através da técnica de retalho estendido associado ao uso do Mucograft. PerioNews 2012;6(3):247-51.
- Lorenzo R, García V, Orsini M, Martin C, Sanz M. Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 2012;23(3):316-24.
- Cardaropoli D, Tamagnone L, Rolfredo A, Gaveglio L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: a randomized controlled clinical trial. J Periodontol 2012;83(3):321-8.
- Schmitt CM, Moest T, Lutz R, Wehrhan F, Neukam FW, Schlegel KA. Long-term outcomes after vestibuloplasty with a porcine collagen matrix (Mucograft) versus the free gingival graft: a comparative prospective clinical trial. Clin Oral Implants Res 2016;27(11):e125-e133.
- Froum SJ, Khouly I, Tarnow DP, Froum S, Rosenberg E, Corby P et al. The use of xenogeneic collagen matrix at the time of implant placement to increase the volume of buccal soft tissue. Int J Periodontics Restorative Dent 2015;35(2):179-89.
- Pabst AM, Wagner W, Kasaj A, Gebhardt S, Ackermann M, Astolfo A et al. Synchrotron-based X-ray tomographic microscopy for visualization of three-dimensional collagen matrices. Clin Oral Investig 2015;19(2):561-4.
- Sclar A. The Bio-Col technique. In: Sclar A (ed). Soft Tissue and Esthetic Considerations in Implant Therapy. Chicago: Quintessence, 2003. p.75-112.
- Berk H. Reimplantação. In: Berk H(ed). Como salvar um dente. São Paulo: Editora Santos, 2011. p.89-107.
- Yukna R, Tow HD, Caroll PB, Vernino AR, Bright RW. Comparative clinical evaluation of freeze-dried skin allografts and autogenous gingival grafts in humans. J Clin Periodontol 1977;4(3):191-9.
- Ghannaati S, Schlee M, Webber MJ, Willershausen I, Barbekc M, Balic E et al. Evaluation of the tissue reaction to a new bilayered collagen matrix in vivo and its translation to the clinic. Biomed Mater 2011;6(1):015010.
- Willershausen I, Barbeck M, Boehm N, Sader R, Willershausen B, Kirkpatrick CJ et al. Non-cross-linked collagen type I/III materials enhance cell proliferation: in vitro e in vitro evidence. J Appl Oral Sci 2014;22(1):29-37.
- Kasaj A, Levin L, Stratul SI, Götz H, Schlee M, Rütters CB et al. The influence of various rehydration protocols on biomechanical properties of different acellular tissue matrices. Clin Oral Investig 2016;20(6):1303-15.
- Rocchietta I, Schupbach P, Ghezzi C, Maschera E, Simion M. Soft tissue integration of a porcine collagen membrane: an experimental study in pigs. Int J Periodontics Restorative Dent 2012;32(1):e34-40.
- Jung RE, Hürzeler MB, Thoma DS, Khraisat A, Hämmerle CHF. Local tolerance and efficiency of two prototype collagen matrices to increase the width of keratinized tissue. J Clin Periodontol 2011;38(2):173-9.
- Morton D, Chen ST, Martin WC, Levine RA, Buser D. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants 2014;29(suppl.):216-20.
- Sullivan H, Atkins J. Free autogenous gingival grafts. I. Principles of successful grafting. Periodontics 1968;6(3):121-9.
- Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000 1996;11:18-28.
- Degidi M, Nardi D, Piattelli A. One abutment one time: non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin Oral Implants Res 2011;22(11):1303-7.
- Wadhwani C, Piñeyro A. Technique for controlling the cement for an implant crown. J Prosthet Dent 2009;102(1):57-8.
- Nunes MP, Mazaro JVQ, Ogliari PV, Vedovatto E, Muglia VA, de Alexandre RS et al. Implantação e carregamento imediato unitário na região posterior – relatos de casos clínicos com acompanhamento de um a quatro anos. ImplantNewsPerio 2016;1(2):277-87.