RESUMO
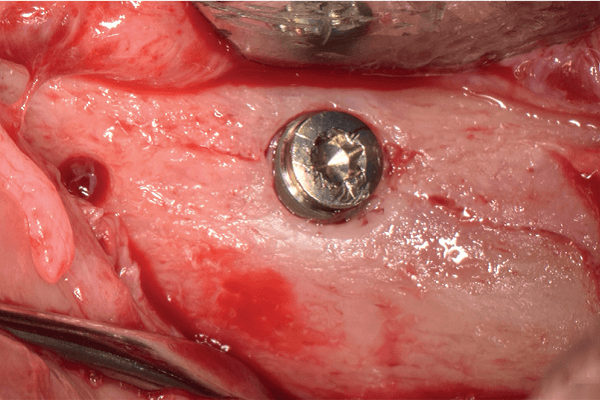
A técnica de lateralização in-block consiste de uma adicional alternativa de mobilização do nervo alveolar inferior, com acompanhamento de longo prazo clínico e tomográfico de 54 casos, com mínimo de três anos de acompanhamento e tempo médio de follow-up de três a dez anos. Diante dos resultados apresentados ao longo deste tempo, a técnica vem demonstrando ser uma opção previsível e eficiente no tratamento das atrofias posteriores de mandíbula, evitando o uso de enxertos ou biomateriais de alto custo, bem como exodontias múltiplas de dentes anteriores saudáveis para a realização de reabilitações totais inferiores. As situações clínicas com menos de 4 mm de altura óssea alveolar, limite para o tratamento com implantes extracurtos, tornam-se a principal indicação da lateralização in-block, que se caracteriza principalmente pela modificação da via de acesso ao nervo alveolar inferior (NAI), permitindo sua ampla visualização durante o procedimento e com a consequente manipulação mais previsível e delicada do nervo. O uso da piezocirurgia e o reposicionamento do bloco ósseo ao leito original permite a recomposição do contorno mandibular basal e a ideal cicatrização do implante instalado. Apesar da técnica ser considerada relativamente sensível e necessitar de desenvolvimento e evolução continuada, podemos observar que os resultados obtidos até então vêm consolidando sua indicação na reabilitação das condições de severa atrofia mandibular posterior.
Palavras-chave – Nervo mandibular; Implantação dentária; Cirurgia bucal; Lateralização do nervo alveolar inferior; Mandíbula atrófica.
ABSTRACT
The in-block lateralization technique consists of an additional alternative of inferior alveolar nerve mobilization, with long-term clinical and tomographic follow-up of 54 cases with a minimum of 3 years of follow-up and mean follow-up time of 3 to 10 years. Given the results presented over this time, the technique has proven to be a predictable and efficient option in the treatment of posterior jaw atrophies, avoiding the use of grafts or high-cost biomaterials, as well as multiple extractions of healthy anterior teeth to perform lower total rehabilitation. Clinical situations with less than 4 mm of alveolar bone height, the limit for treatment with extra-short implants, becomes the main indication of in block lateralization which is characterized mainly by the modification of the access route to the inferior alveolar nerve (IAN), allowing its wide visualization during the procedure and with the consequent more predictable and delicate manipulation of the nerve. The use of piezosurgery and the repositioning of the bone block to the original bed allows the recomposition of the basal mandibular contour and the ideal healing of the implant installed. Although the technique is considered relatively sensitive and requires continuous development and evolution, we can observe that the results obtained so far have been consolidating its indication in the rehabilitation of conditions of severe posterior mandibular atrophy.
Key words – Mandibular nerve; Dental implants; Surgery oral; Inferior alveolar nerve lateralization; Atrophic mandible.
Referências
- Ikeda K, Ho KC, Nowicki BH, Haughton VM. Multiplanar MR and anatomic study of mandibular canal. AJNR Am J Neuroradiol 1996;17(3):579-84.
- Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol 2006;77(12):1933-43.
- Browaeys H, Bouvry P, De Bruyn H. A literature review of biomaterials in sinus augmentation procedures. Clin Implant Dent Relat Res 2007;9(3):166-77.
- Gatti F, Gatti C, Tallarico M, Tommasato G, Meloni SM, Chiapasco M. Maxillary sinus membrane elevation using a special drilling system and hydraulic pressure: a 2-year prospective cohort study. Int J Periodontics Restorative Dent 2018;38(4):593-9.
- Fornell J, Johansson LÅ, Bolin A, Isaksson S, Sennerby L. Flapless, CBCT-guided osteotome sinus floor elevation with simultaneous implant installation. I: radiographic examination and surgical technique. A prospective 1-year follow-up. Clin Oral Implants Res 2012;23(1):28-34.
- Trajkovski B, Jaunich M, Müller WD, Beuer F, Zafiropoulos GG, Houshmand A. Hydrophilicity, viscoelastic, and physicochemical properties variations in dental bone grafting substitutes. Materials (Basel) 2018;11(2):215.
- Jensen T, Schou S, Stavropoulos A, Terheyden H, Holmstrup P. Maxillary sinus floor augmentation with Bio-Oss or Bio-Oss mixed with autogenous bone as graft: a systematic review. Clin Oral Implants Res 2012;23(3):263-73.
- Korenkov AV, Sikora VZ. Computed tomographic evaluation of the healing of experimental defect of a long bone of the skeleton after implantation into its cavity osteoplastic material “Cerabone”. Georgian Med News 2015;(238):89-93.
- Gerzson AS, Bravo MM, Teixeira GS, Lopes LAZ. Atrophic jaw posterior rehabilitation with short and extra-short implants: two cases report. J Clin Dent Res 2017;14(4):74-85.
- Anitua E, Orive G, Aguirre JJ, Andía I. Five-year clinical evaluation of short dental implants placed in posterior areas: a retrospective study. J Periodontol 2008;79(1):42-8.
- Al-Johany SS, Al Amri MD, Alsaeed S, Alalola B. Dental implant length and diameter: a proposed classification scheme. J Prosthodont 2017;26(3):252-60.
- Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006;21(2):275-82.
- Sivolella S, Stellini E, Testori T, Di Fiore A, Berengo M, Lops D. Splinted and unsplinted short implants in mandibles: a retrospective evaluation with 5 to 16 years of follow-up. J Periodontol 2013;84(4):502-12.
- Pjetursson BE, Heimisdottir K. Dental implants – are they better than natural teeth? Eur J Oral Sci 2018;126(suppl.1):81-7.
- Clark D, Levin L. In the dental implant era, why do we still bother saving teeth? J Endod 2019;45(12S):S57-S65.
- Vetromilla BM, Moura LB, Sonego CL, Torriani MA, Chagas Jr. OL. Complications associated with inferior alveolar nerve repositioning for dental implant placement: a systematic review. Int J Oral Maxillofac Surg 2014;43(11):1360-6.
- Palacio García-Ochoa A, Pérez-González F, Negrillo Moreno A, Sánchez-Labrador L, Cortés-Bretón Brinkmann J, Martínez-González JM et al. Complications associated with inferior alveolar nerve reposition technique for simultaneous implant-based rehabilitation of atrophic mandibles. A systematic literature review. J Stomatol Oral Maxillofac Surg 2020;121(4):390-6.
- Abayev B, Juodzbalys G. Inferior alveolar nerve lateralization and transposition for dental implant placement. Part I: a systematic review of surgical techniques. J Oral Maxillofac Res 2015;6(1):e2.
- Tomazi MA, Gerzson AS, Menuci Neto A, da Costa ALP. In-block lateralization as a new technique for mobilization of the inferior alveolar nerve: a technique case series. J Oral Implantol 2021;47(4):333-41.
- Pavlíková G, Foltán R, Horká M, Hanzelka T, Borunská H, Sedý J. Piezosurgery in oral and maxillofacial surgery. Int J Oral Maxillofac Surg 2011;40(5):451-7.
- Pereira CC, Gealh WC, Meorin-Nogueira L, Garcia-Júnior IR, Okamoto R. Piezosurgery applied to implant dentistry: clinical and biological aspects. J Oral Implantol 2014;40:401-8.
- Liu J, Hua C, Pan J, Han B, Tang X. Piezosurgery vs conventional rotary instrument in the third molar surgery: a systematic review and meta-analysis of randomized controlled trials. J Dent Sci 2018;13(4):342-9.
- Gerzson AS, Weissheimer T, Soares N, Pagnoncelli RM, da Rosa RA. Controle farmacológico da dor pós-operatória na odontologia: uma revisão. RSBO 2021;18(1):107-14.
- Marx RE. Bone and bone graft healing. Oral Maxillofac Surg Clin North Am 2007;19(4):455-66.
- Bigham-Sadegh A, Oryan A. Basic concepts regarding fracture healing and the current options and future directions in managing bone fractures. Int Wound J 2015;12(3):238-47.
- Adell R. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10(6):387-416.
- Capelli M, Zuffetti F, Del Fabbro M, Testori T. Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: a multicenter clinical study. Int J Oral Maxillofac Implants 2007;22(4):639-44.
- Del Fabbro M, Bellini CM, Romeo D, Francetti L. Tilted implants for the rehabilitation of edentulous jaws: a systematic review. Clin Implant Dent Relat Res 2012;14(4):612-21.
- Gerzson AS, Lauxen BL, Weissheimer T, Paludo E, Lopes LAZ. Assessment of quality of life in total edentulous patients rehabilitated with implants and fixed prosthesis. Braz J Oral Sci 2022;21:e225686.